
People struggling with substance abuse were once, and sometimes still are, judged harshly. Today, we know addiction is a disease, just as cancer, diabetes and other common ailments are. The National Institute of Drug Abuse, respected institutions like the American Medical Association and studies published in notable publications all define addiction as a disease.
According to the National Institute of Drug Abuse, addiction, also called substance use disorder, is a “chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite harmful consequences.”
The science of addiction
So, how does it happen? What’s the science behind it? Let’s first refresh our memory of the limbic system. This part of the brain is responsible for our basic survival instincts, such as eating, finding shelter, and caring for our young. When we participate in such activities, our brain triggers the release of a neurotransmitter called dopamine. According to AddictionPolicy.org’s article on the science of addiction, it not only makes us feel good but the feeling is also sent to the area of the brain that records memory, causing people to repeat the behavior in the future.
So, what happens when drugs are involved? Drugs trigger that same part of the brain (the reward system). According to Shatterproof.org’s article about the science of addiction, “When someone takes a drug, their brain releases extreme amounts of dopamine—way more than gets released as a result of a natural pleasurable behavior.” As a result, the brain overcompensates and greatly reduces the amount of dopamine it’s producing in an effort to normalize the high levels the drugs have triggered. When drug use is repeated, the brain adapts, scaling back its sensitivity to dopamine. This tolerance means that it takes more drugs for the user to reach the same “high”. That’s not the only effect though. Since these same circuits control our ability to take pleasure from everyday rewards like food and spending time with loved one, drug users also experience reduced pleasure from those ordinary activities.
Treatment and healing
Once someone is addicted, they experience painful withdrawal symptoms and cravings take over, causing them to act compulsively and make potentially destructive decisions. While addiction is considered a disease—one that can’t be cured—it can be treated and the risk factors can be managed.
“Thankfully we are much more educated about addiction than we once were,” said Bevan Allen, director of operations at Compass Mark.
“We know that the behaviors that hurt the individual and those who love them are symptoms of the brain disease and that it medically requires treatment and support over time to improve those damaged connections.”
“One important piece of the science behind addiction that drives our work at Compass Mark is acknowledging that everyone has an individual level of risk for addiction.”
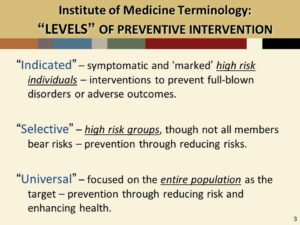
“If you’ve ever wondered how one person can end up with a use problem, when others can just stop using because they decide to, you were observing risk levels,” Allen explained. “Being genetically predisposed to addiction, experiencing mental health challenges or even experiencing trauma can increase an individual’s risk for addiction.”
Compass Mark’s key strategy for reducing risk is helping people build up “protective factors” to counteract the risk factors.
“Having someone you trust, belonging to a group, having healthy activities and avoiding risky opportunities that can take you off track, are often what’s needed to correct course,” Allen said. “Addiction is not something we are powerless against but is a problem we can all solve together. Like heart health or diabetes, we can manage the risk to protect our health from the disease of addiction.”